The democratisation of SME credit in The Philippines: Why We Invested in ProCredit
7 March, 2024
Empowering Indonesia’s Poultry Farmers: Why We Invested in Chickin
24 October, 2024Reimagining Women’s Health: Why We Invested in Kindred Health
2 August, 2024
Beyond sexual and reproductive health
Of the many treasures housed in The Royal Belgian Institute of Natural Sciences in Brussels, one of the most-prized is the small, brown bone roughly the size of a pencil. The Ishango Bone dates back more than 20,000 years, and its surface is covered in tally marks that have been the subject of fevered speculation. Some archeologists argue that the bone is evidence of man’s early understanding of mathematics, or perhaps man’s first attempt at a lunar calendar. In 1991, math educator Claudia Zaslavsky proposed a slightly different interpretation. “Tell me,” she quipped, “what man needs to know when 28 days have passed? I suspect that this is woman’s first attempt at a calendar.”
FIGURE 1 - Period trackers have come a long way in 20,000 years
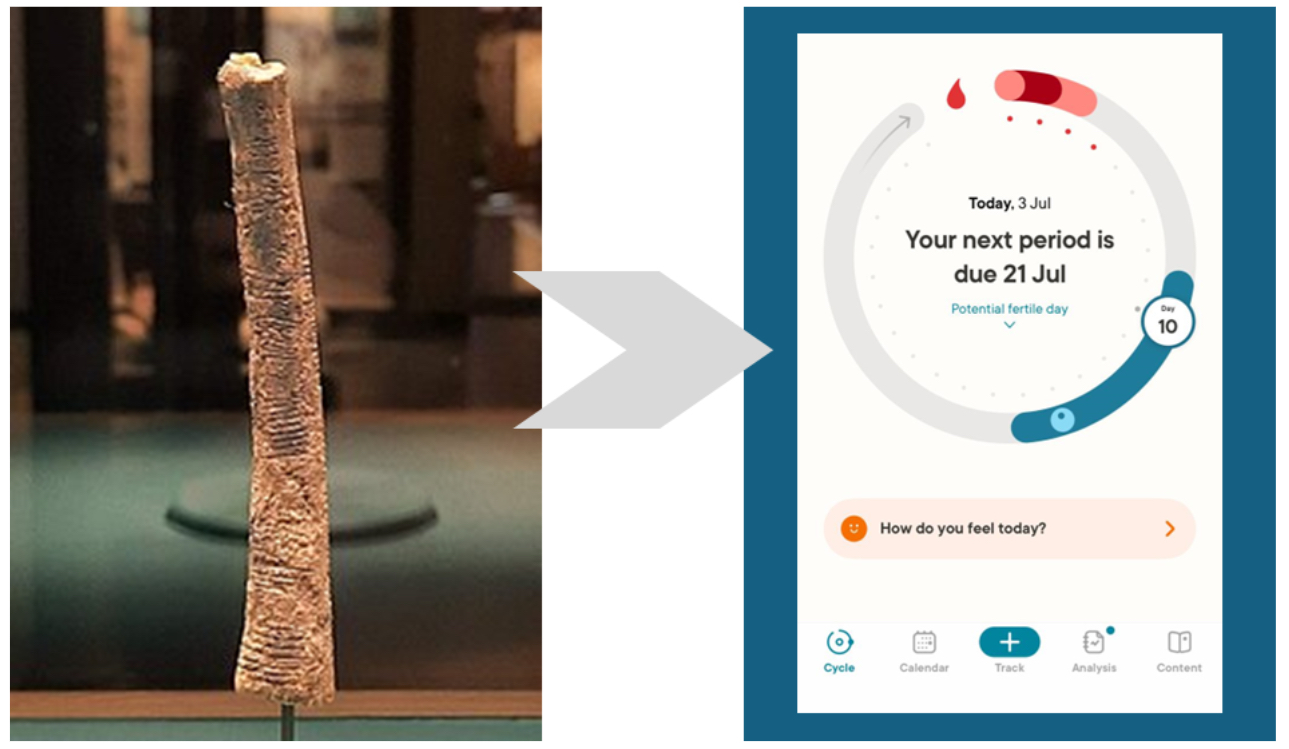
Period trackers (if the Ishango Bone really was one) have come a long way since then, but Zaslavsky highlights a basic truth. Men’s and women’s bodies are fundamentally different, beginning with the fact that women have menstrual cycles, and men don’t. So it’s natural that the “femtech revolution” in the startup world started with sexual and reproductive health, with the highest-profile companies like Clue and Flo being anchored on period tracking apps.
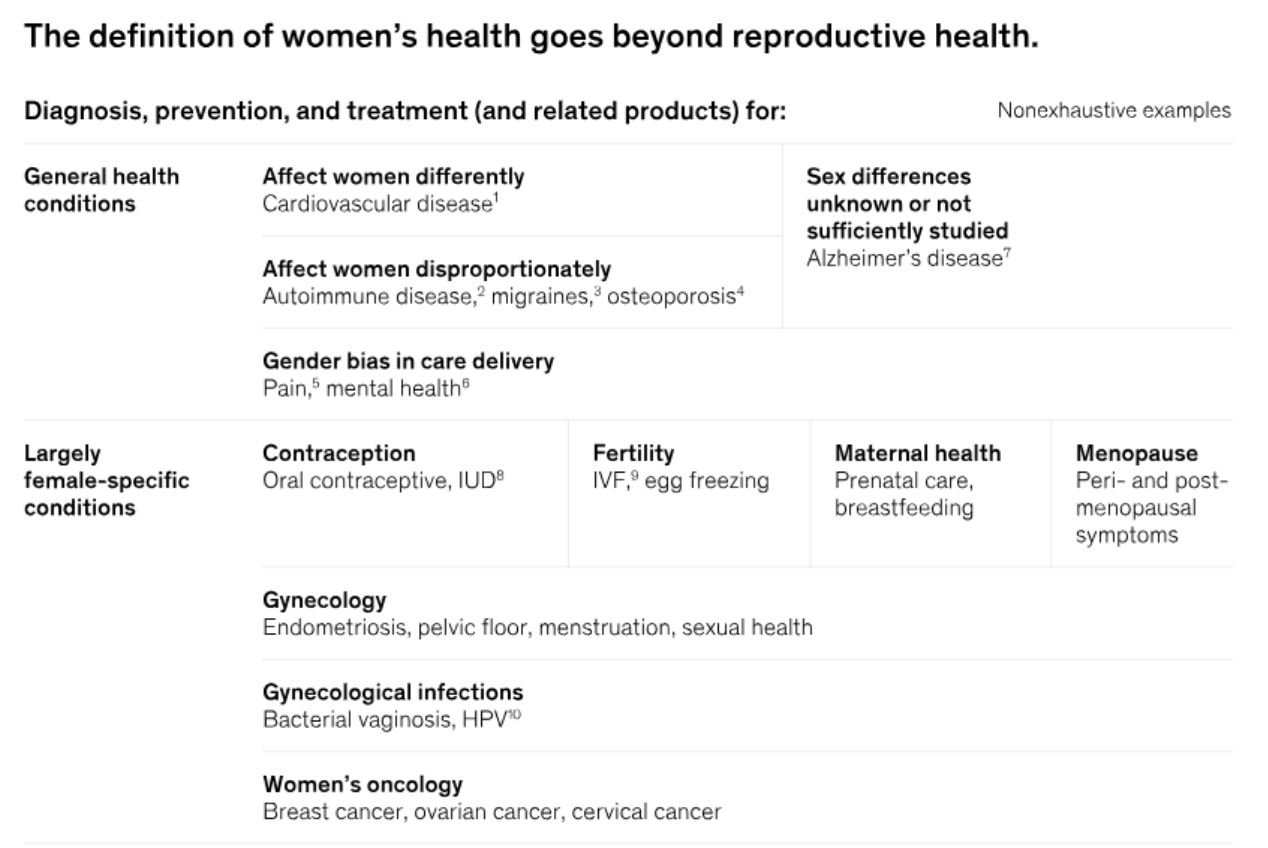
But we are now starting to understand that sex-based differences “influence all tissues, organs, and bodily functions” and have implications far beyond our respective reproductive roles. This means that we need to think about disease prevention, diagnosis and treatment differently in men vs. women. For a range of historical reasons, medical research has largely used men as test subjects, on the assumption that findings could be generalised across to women, which has created a massive gender-based blind spot in healthcare data that stretches back decades. (For the historical reasons why, we’ve included a short footnote at the end of this article.) Diagnosis criteria for heart attacks have been built using symptoms that commonly manifest in men - so women are 50% more likely than men to be misdiagnosed, even though cardiovascular disease is one of the top killers of both men and women. Or take testing for medical devices. Hip implants are known to fail 2x more often in women than in men, because men’s hips bear weight differently from women’s. Or drug testing. Early research indicates that women may metabolise up to 70-80% of all prescribed drugs differently from men - and yet gender-specific dosing instructions are absent for the vast majority of medications today. As a result, women are 50-75% more likely to experience adverse drug reactions. Famously, the FDA halved the dosing recommendation for women for the sedative zolpidem (aka Ambien) in 2013 - a full 16 years after the drug had come to market - because at the standard dose, zolpidem levels in women remain high enough the next morning to impair alertness. That’s a lot of drug-impaired women drivers over many years - and think how many other Ambiens might be out there.
In fact, McKinsey estimates that sexual and reproductive health (SRH) and maternal, newborn and child health (MNCH) account for only 5% of a woman’s health burden - with another 56% coming from health conditions that are more prevalent and/or manifest differently in women. Accordingly, the opportunity set in women’s health extends far beyond where femtech has reached today - and that is the reason why we are so excited about our investment in Kindred Health.
Sexual and reproductive health (SRH) and maternal, newborn and child health (MNCH) account for only 5% of a women’s health burden - with another 56% coming from health conditions that are more prevalent and/or manifest differently in women. Accordingly, the opportunity set in women’s health extends far beyond where femtech has reached today.
McKinsey’s framework for a new definition of women’s health
Enter Kindred Health
All this points to the enormous possibilities that could be unlocked if healthcare was reimagined for female patients - which is exactly what our newest portfolio company, Kindred Health, is doing in the Philippines. Kindred doesn’t limit itself to offering ob-gyn or sexual wellness services - it simply offers healthcare, just with the needs and specificities of a female patient in mind. You might show up at the clinic because you have a gynaecological issue - but you could also show up for a flu shot, because you have a cold, or because you need an annual health checkup.
What Kindred is doing is clearly striking a chord. Kindred started with one clinic in Taguig City in the Philippines, and demand has been overwhelming from the get-go. That one clinic alone has served more than 20,000 women in a little over a year, with more than 40% of patients coming back for return visits. The patients come back because they are receiving care that is designed for them, and not someone else, and because Kindred is proving that healthcare can be a warm, inviting, positive and still affordable experience, rather than a shame-filled, clinical one.
FIGURE 2 - What low-cost “lying-in centers” for deliveries look like in the Philippines

Kindred’s goal is to expand its clinic network across the Philippines. Its second clinic is already slated to open in August of this year, and plans are in place for several more locations. To reach patients in the more remote parts of the country, Kindred replicated its clinic experience in their Kindred Karavan, a moving van that the team repurposed to create a mobile clinic. But as Kindred’s operations become larger and more complex, its systems will have to grow up alongside so that patient journeys are consistent and the care they receive is of high quality no matter where they go, and they will have to rely more heavily on technology to communicate with, triage and track their patients. Luckily, the Kindred team is being spearheaded by founder and CEO Jess de Mesa and COO Charmaine Isabel Lim, both former nurses who also bring with them experience in scaling up operations in e-commerce and offline chains. Jess comes from Zalora, where she served as commercial director, while Charmaine Isabel comes from Easy Franchise, where her job was to roll out franchises across the country.
How Kindred fits into a VC fund mandate
Of course, VCs are usually in the business of investing in innovation, not funding offline clinic chains. The thing is, sometimes innovations don’t have to be large to start a huge transformation. The funds from this round of investment will go towards scaling up Kindred’scustomer-facing and internal systems, and to ensure that patient data is captured in as granular and clinically useful a way as possible.
It’s a Silicon Valley truism to say that the value is in the data. In fact, last year, we wrote a whole article on how to think about the value of data in healthcare. Lots of VC funding has gone towards period trackers and symptom checking apps because they are great hooks for capturing patient data, but in most instances these apps have struggled to monetize. Very frequently, tracking and checking is also where the patient journey ends - leaving users with an identified problem but without the care that they know they need.
The best way to capture the value of data is to be able to use it yourself. The difference is, the data that patients put into their Kindred app will go towards enabling their Kindred doctors to have far more context about their health status and historical symptoms, and the doctors will also be able to far better coordinate care across different medical specialisations, because that is what Kindred’s processes are designed around.
The best way to capture the value of data is to be able to use it yourself. That’s why Kindred is building an ecosystem of care. Kindred started with one clinic and a simple appointment booking app, but the app will evolve to include tracking for menstrual cycles, moods, symptoms, and medication. The difference is, the data that patients put into their Kindred app will go towards enabling their Kindred doctors to have far more context about their health status and historical symptoms. And they will also be able to far better coordinate care across different medical specialisations, because that is what Kindred’s processes are designed around. That kind of data will also help Kindred to launch healthcare subscription plans to ensure that its patients can achieve good healthcare outcomes at an affordable cost, a very welcomed development in a country where the government healthcare plan (PhilHealth) covers few women’s health issues and where private insurance penetration (largely through HMOs) is under 6%.
Finally, the big, hairy, audacious goal is that the data that Kindred collects can one day go towards designing a healthcare system that works just as well for women as for men - whether that’s to better understand how to manage drug dosing for women, or how menstrual cycles affect the presentation of disease symptoms, or to enable higher female participation in clinical trials - not just in the Philippines, but everywhere. Think about what gains in healthcare efficacy for women would mean for insurance losses, and for healthcare access and affordability across the board.
The big, hairy, audacious goal is that the data that Kindred collects can one day go towards designing a healthcare system that works just as well for women as for men. Think about what gains in healthcare efficacy for women would mean for insurance losses, and for healthcare access and affordability across the board.
But what about all that capex?
Back in 2020, we all thought that Covid would bring about the age of telemedicine. The user base of telemedicine companies in Southeast Asia grew by 40-150% in the space of a year, and to this day telemedicine is far more widely adopted in this region than would have been possible without a catalyst like the pandemic. But as the world has emerged from lockdowns, what we’ve discovered is that telemedicine works best as a component in a system of care, and that has to include physical clinics for physical bodies.
The growth potential of clinic networks remains exponential in countries like the Philippines where healthcare infrastructure is severely underinvested. A successful healthcare entrepreneur we once met scoffed when we asked him (pre-pandemic) what he thought of telemedicine. “Why would I waste my time fooling around with stuff like that,” he asked, “when I know that every clinic I can build will be full to capacity in a matter of months? What’s the point of nice-looking telemedicine apps that can address a sliver of healthcare issues when what this country needs is more doctors, more nurses and more clinics?” While we may not necessarily agree with everything in that statement, the point is that, the pent-up need for quality healthcare in countries like the Philippines means that telemedicine-integrated, tech-forward, data-driven clinic networks can drive exponential returns.
The pent-up need for quality healthcare in countries like the Philippines means that telemedicine-integrated, tech-forward, data-driven clinic networks can drive exponential returns.
And just as telemedicine fits into a broader healthcare system, in some situations, VC can best drive large-scale transformation as part of a broader system of funding and capital. The question that we asked ourselves when we considered our investment was whether our capital could grow Kindred to a stage where they could unlock other forms of funding to further fuel their growth and capture those types of returns. And with the right deal structure, the answer is yes.
In conclusion
McKinsey estimates that the global gender health gap is equivalent to 75 million disability-adjusted life years, which, if closed, could add $1 trillion to the global economy annually by 2040. It is an opportunity just waiting to be picked - which is why we’re so excited to partner with Jess, her cofounder Abet, COO Charmaine Isabel, and CMO Dr. Judith Peralta to go after the opportunity. Together with our co-shareholders Kaya Founders, Pulse63 and KSR Ventures, we’re reimagining healthcare for the other 50%.